
Chapter 29: Reproduction and Embryonic Development
29.1 How Animals Reproduce
Asexual Versus Sexual Reproduction
Animals can reproduce sexually or asexually.
Asexual reproduction involves only one parent.
Offspring in asexual reproduction are usually genetically identical to the parent.
Sexual reproduction involves two parents.
Genetic material is shuffled in sexual reproduction.
Offspring in sexual reproduction usually have combinations of genes that are not like those of either parent.
Forms of Asexual Reproduction
Asexual reproduction occurs in hydra, a type of cnidarian.
Hydras can reproduce by budding, where a new individual arises as an outgrowth of the parent.
Many flatworms can constrict into two halves, and each half regenerates to become a new individual.
Fragmentation, followed by regeneration, is seen among sponges, echinoderms, and corals.
Chopping up a sea star does not kill it; instead, each fragment can grow into another animal if a portion of the oral disk is retained with the cut fragment.
Parthenogenesis is a modification of sexual reproduction in which an unfertilized egg develops into a complete individual.
In honeybees, the queen bee can fertilize eggs or allow eggs to pass unfertilized as she lays them.
The fertilized eggs become diploid females called workers, and the unfertilized eggs become haploid males called drones.
Parthenogenesis is also observed in some fish (including sharks) and in a number of amphibian and reptile species.

Sexual Reproduction
Sexual reproduction in animals involves the production of gametes in specialized organs called gonads.
Male gonads are called testes and produce sperm, while female gonads are called ovaries and produce eggs.
Germ cells become specialized for this purpose during early development.
Fertilization usually occurs when the egg of one parent is fertilized by the sperm of another, resulting in a zygote.
Even hermaphroditic earthworms frequently undergo cross-fertilization.
In some animals, the gonads may change function due to environmental conditions.
Aquatic animals often practice external fertilization, while internal fertilization involves copulation.
Animals either produce eggs or give birth to live offspring.
Oviparous animals lay eggs that will hatch after ejection from the body, while ovoviviparous animals retain the eggs in the body until they hatch.
Viviparous animals produce living young and provide nourishment during development via the placenta and mammary glands.
The evolution of the placenta allowed the developing offspring to exchange materials with the mother internally.

29.2 Human Reproduction
The human reproductive system has two components:
Gonads (testes in males and ovaries in females) produce gametes and sex hormones.
Accessory organs conduct gametes and house the embryo/fetus in females.
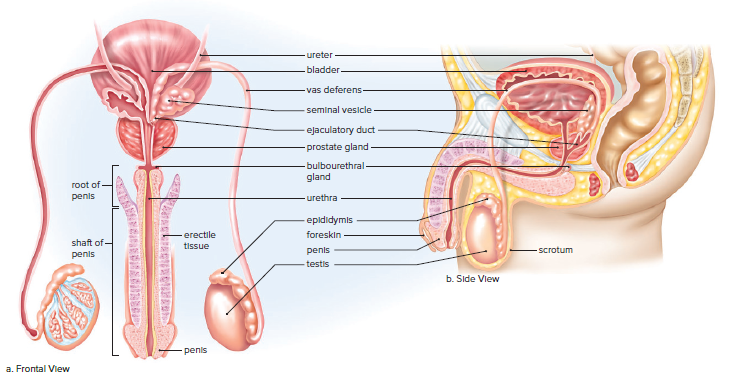
Male Reproductive System
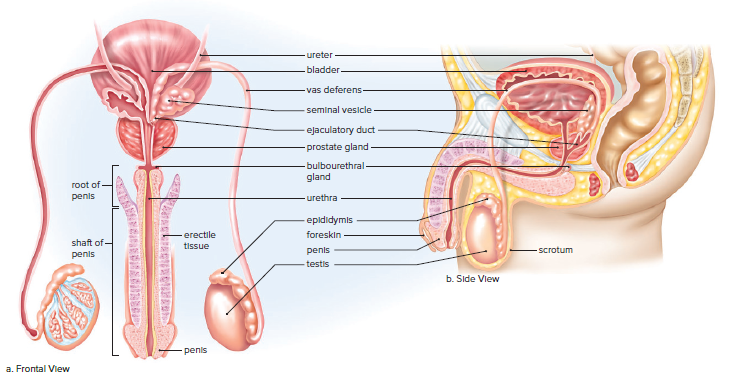
The male reproductive system includes the testes, epididymis, vas deferens, urethra, penis, seminal vesicles, prostate gland, and bulbourethral glands.
The testes produce sperm and testosterone.
The epididymis stores and matures sperm.
The vas deferens transports sperm to the ejaculatory duct.
The ejaculatory duct joins the urethra, which carries semen out of the body.
The penis is the male organ for sexual intercourse and urination.
Erection is caused by increased blood flow to the penis.
Semen is a thick, whitish fluid that contains sperm and secretions from the seminal vesicles, prostate gland, and bulbourethral glands.
Ejaculation is the expulsion of semen from the penis.
Orgasm is the climax of sexual stimulation.
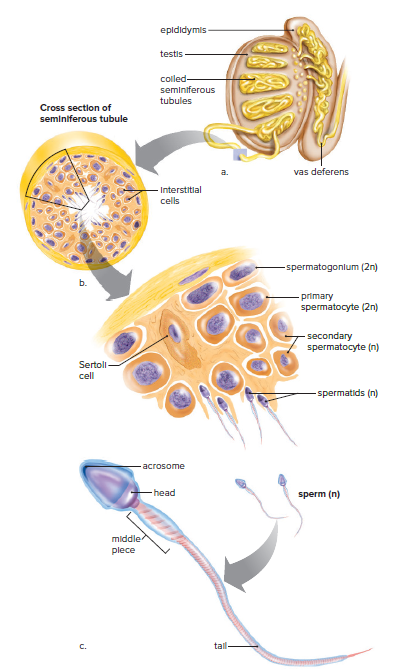
The Testes
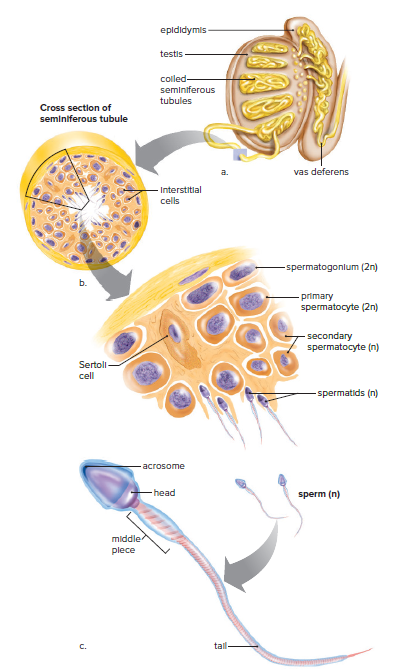
The testes are composed of lobules, each of which contains one to three seminiferous tubules.
The seminiferous tubules are where sperm are produced.
Sperm production is a process called spermatogenesis.
Spermatogenesis involves reducing the chromosome number from diploid (2n) to haploid (n).
Sertoli cells support, nourish, and regulate the production of sperm.
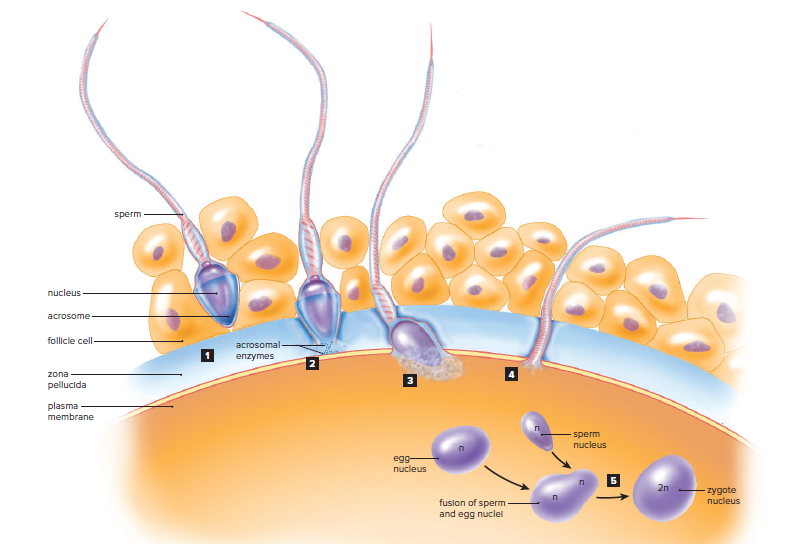
A sperm has three distinct parts: a head, a middle piece, and a tail.
The head contains a nucleus and an acrosome.
The acrosome contains digestive enzymes that help the sperm penetrate the egg's outer membrane.
The tail is a flagellum that allows the sperm to swim.
The middle piece contains mitochondria that produce energy for the sperm.
A normal human male ejaculates 40 million sperm per milliliter of semen.
Only 100 sperm ever reach the vicinity of the egg, and only one sperm normally enters the egg.
Hormonal Regulation in Males
The hypothalamus secretes GnRH, which stimulates the anterior pituitary to produce gonadotropic hormones.
Both males and females have two gonadotropic hormones: FSH and LH.
In males, FSH promotes spermatogenesis in the seminiferous tubules.
LH controls the production of testosterone by the interstitial cells.
Testosterone is essential for the normal development and functioning of the sexual organs and necessary for the maturation of sperm.
Testosterone brings about and maintains male secondary sex characteristics.
Males are generally taller than females and have broader shoulders and longer legs relative to trunk length.
Testosterone causes males to develop noticeable hair on the face, chest, and occasionally other regions of the body, such as the back.
Testosterone leads to the receding hairline and contributes to pattern baldness.
Testosterone is responsible for greater muscular development in males.
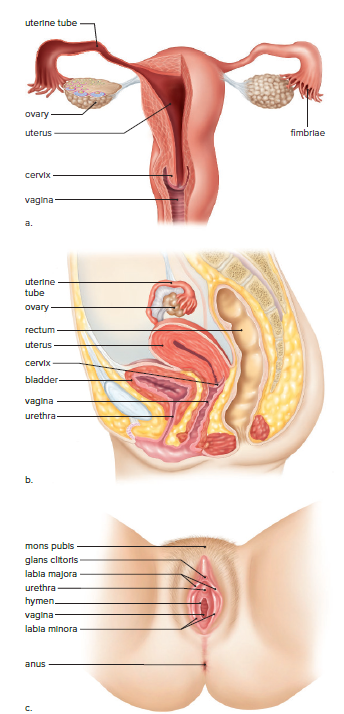
Female Reproductive System
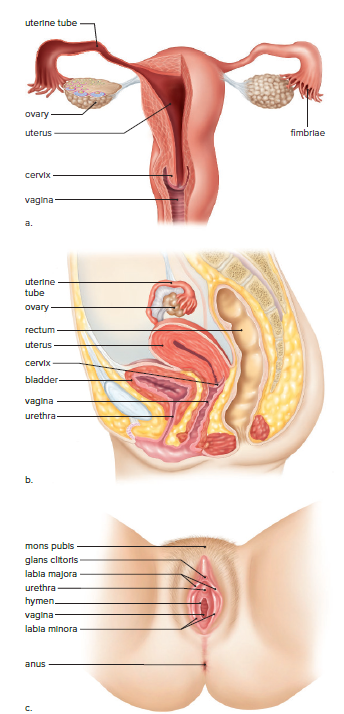
The human female reproductive system includes:
Ovaries
Uterine tubes (oviducts or fallopian tubes)
Uterus
Vagina
The uterine tubes:
Extend from the ovaries to the uterus.
Have fingerlike projections called fimbriae that sweep over the ovaries.
Sweep an oocyte into the uterine tube during ovulation.
Fertilization occurs in the first one-third of the uterine tube.
The developing embryo is propelled to the uterus by ciliary movement and tubular muscle contraction.
The Uterus:
Thick-walled, muscular organ.
Size and shape of an inverted pear.
The narrow end is called the cervix.
The embryo completes its development after embedding itself in the uterine lining (endometrium.)
The vagina:
Tube at a 45° angle with the body’s vertical axis.
The mucosal lining lies in folds, allowing it to expand.
Serves as the birth canal and facilitates sexual intercourse.
The external genital organs (vulva) include:
Mons pubis.
Labia minora and labia majora.
Clitoris (homologous to the penis of males.)
Hymen (thin membrane that partially obstructs the vaginal opening and has no apparent biological function.)
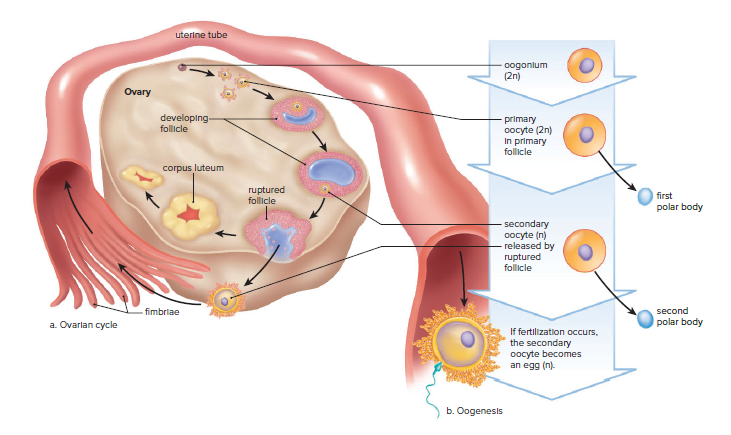
The Ovaries
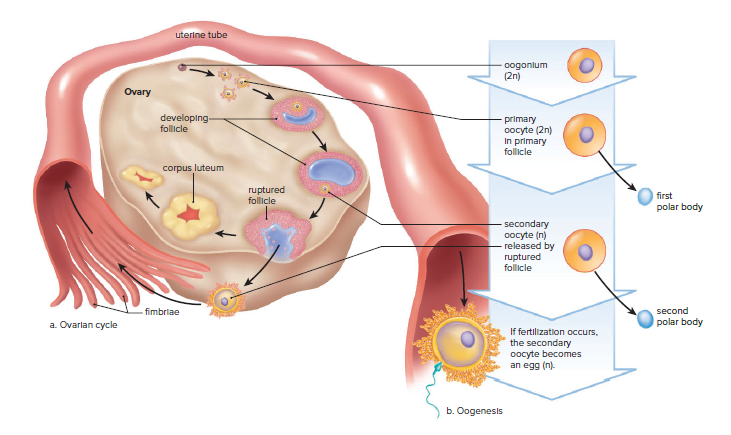
Oogenesis:
An oogonium in the ovary gives rise to an oocyte surrounded by epithelium, forming a primary follicle.
At birth, a female has as many as 2 million primary follicles, but the number reduces to 300,000-400,000 by puberty.
Only about 400 primary follicles ever mature and produce a secondary oocyte.
The mature follicle bursts, releasing the secondary oocyte surrounded by follicle cells, which is called ovulation.
Oogenesis is completed when and if the secondary oocyte is fertilized by a sperm.
A follicle that has lost its oocyte develops into a corpus luteum and stays inside the ovary.
If fertilization and pregnancy do not occur, the corpus luteum begins to degenerate after about 10 days.
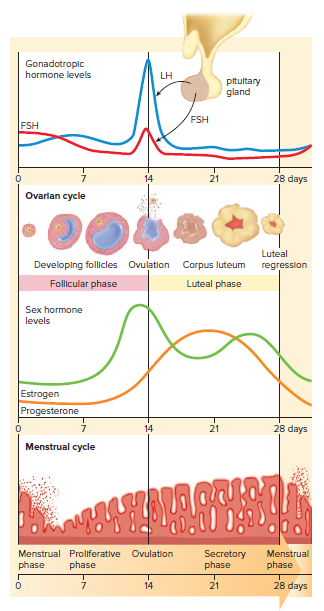
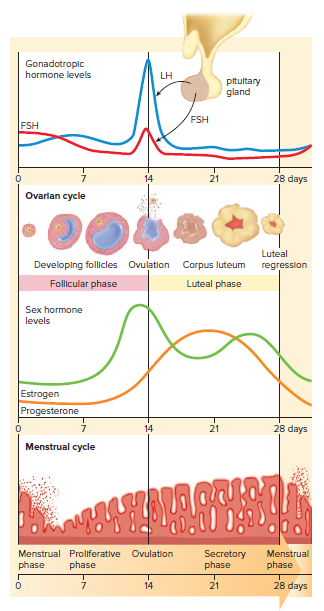
Ovarian Cycle:
The ovarian cycle is controlled by the gonadotropic hormones FSH and LH from the anterior pituitary gland.
During the follicular phase of the cycle, FSH promotes the development of follicles that secrete estrogen.
As the blood level of estrogen rises, it exerts feedback control over FSH secretion, and ovulation occurs.
During the luteal phase of the ovarian cycle, LH promotes the development of a corpus luteum, which secretes primarily progesterone.
As the blood level of progesterone rises, it exerts feedback control over LH secretion, so that the corpus luteum begins to degenerate if fertilization does not occur.
As the luteal phase comes to an end, menstruation occurs.
Menstrual Cycle:
The female sex hormones estrogen and progesterone affect the endometrium of the uterus, causing the series of events known as the menstrual cycle.
The 28-day menstrual cycle in the nonpregnant female is divided into three phases: menstrual, proliferative, and secretory.
During the menstrual phase, female sex hormones are at a low level in the body, causing the endometrium to disintegrate and its blood vessels to rupture.
During the proliferative phase, increased production of estrogen by ovarian follicles causes the endometrium to thicken and become vascular and glandular.
Ovulation usually occurs on day 14 of the 28-day cycle.
Hormonal Regulation in Females
Estrogen and progesterone are female sex hormones.
Estrogen is essential for normal development and functioning of female reproductive organs.
Estrogen is responsible for secondary sex characteristics in females, including body hair and fat distribution.
Females have a more rounded appearance than males due to a greater accumulation of fat beneath their skin.
The pelvic girdle aligns so that females have wider hips than males, and thighs converge at a greater angle toward the knees.
Both estrogen and progesterone are required for breast development.
Menopause occurs between ages 45 and 55 and is the time when ovarian and menstrual cycles cease.
Menopause is not complete until menstruation has been absent for a year.
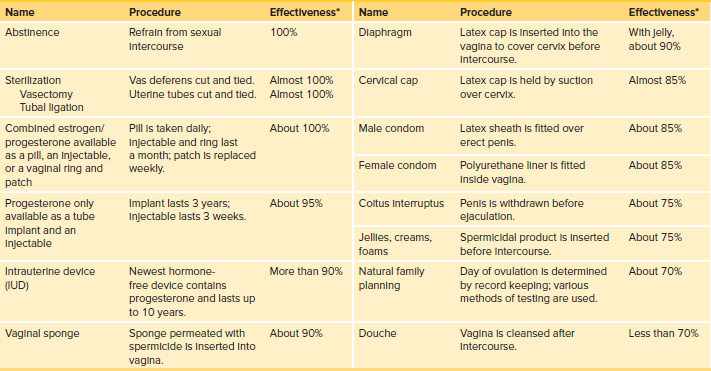
Control of Reproduction
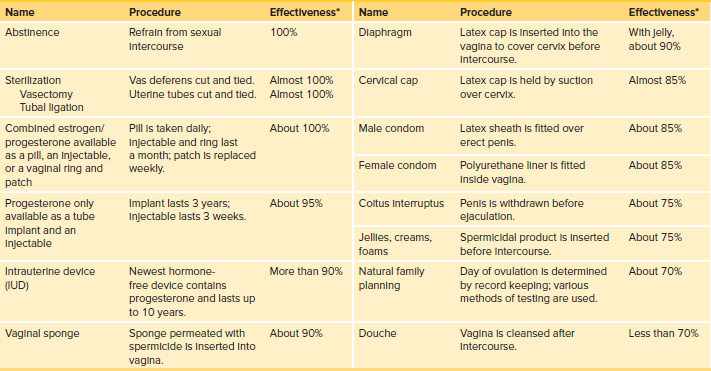
Table 29.1 lists various means of birth control and their rates of effectiveness with consistent and correct usage.
Figure 29.9 illustrates some birth control devices.
Abstinence is a reliable method of birth control that also prevents sexually transmitted diseases.
Oral contraceptives contain estrogen and progesterone, which prevent ovulation and pregnancy. Women taking birth control pills should see a physician regularly due to possible side effects.
Contraceptive implants use synthetic progesterone to prevent ovulation and are available in a single capsule that remains effective for about 3 years.
Contraceptive injections are available as progesterone only or as a combination of estrogen and progesterone and can last from a few weeks to several months.
Barrier methods of birth control, such as condoms, offer some protection against sexually transmitted diseases. Female condoms consist of a large, polyurethane tube with a flexible ring that fits onto the cervix, while male condoms are a latex sheath that fits over the erect penis.
The diaphragm is a soft, latex cup with a flexible rim that lodges behind the pubic bone and fits over the cervix. Each woman must be properly fitted by a physician and used with spermicidal jelly or cream.
The cervical cap is a mini-diaphragm.
An intrauterine device (IUD) is a small piece of molded plastic that is inserted into the uterus by a physician or another qualified health-care practitioner.
Contraceptive vaccines are currently being researched, including a vaccine intended to immunize women against human chorionic gonadotropin (hCG) and a safe antisperm vaccine for women.
Emergency contraception includes approaches to birth control that can prevent pregnancy after unprotected intercourse.
The first FDA-approved medication produced for emergency contraception was a kit called Preven, which includes four synthetic progesterone pills.
Plan B One-Step is up to 89% effective in preventing pregnancy if taken within 72 hours after unprotected sex and is available without a prescription to women aged 17 and older.
Ulipristal acetate (also known as “ella”) was approved for emergency contraception in 2010 and can be taken up to 5 days after unprotected sex.
Mifepristone, also known as RU-486 or the “abortion pill,” can cause the loss of an implanted embryo by blocking the progesterone receptors of endometrial cells.

Infertility
Control of reproduction involves preventing pregnancy and treating infertility.
Infertility is the inability to produce offspring, affecting 1 in 6 couples in America.
Causes of infertility: male (40%), female (40%), or both (20%).
Low sperm count and abnormal sperm are common causes of male infertility.
A sedentary lifestyle, smoking, and alcohol consumption can lead to male infertility.
Female body weight is an important fertility factor.
Normal weight produces the hormone leptin, stimulating follicle formation in ovaries.
Overweight women may have ineffective follicles and no ovulation.
Polycystic ovary syndrome (PCOS) affects 10% of women of childbearing age.
PCOS causes many cysts but no functioning follicles, leading to no ovulation.
Blocked uterine tubes and endometriosis are other causes of female infertility.
Medical intervention can correct some causes of infertility.
Fertility drugs can stimulate ovaries and bring about ovulation.
Assisted reproductive technologies are an option for couples who cannot conceive.
Assisted Reproductive Technologies
Assisted Reproductive Technologies (ART):
Techniques used to increase chances of pregnancy.
Sperm and/or eggs are retrieved from the testes and ovaries.
Fertilization takes place in a clinical or laboratory setting.
Artificial Insemination by Donor (AID):
Sperm is placed in the vagina by a physician.
A woman can be inseminated by her partner's sperm or the donor's sperm.
Helpful for low sperm count, sperm can be collected over time and concentrated.
In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI):
Conception occurs outside the body in a laboratory.
Ultrasound machines are used to spot follicles in ovaries holding immature eggs.
Immature eggs retrieved using a needle.
In IVF, immature eggs are brought to maturity in glassware before adding concentrated sperm.
In ICSI, a single sperm is injected into an egg.
Embryos are transferred to the uterus of a woman in the secretory phase of the menstrual cycle.
Embryos can be tested for genetic disease before use.
Multiple births are common if several embryos are transferred.
Excess embryos may be frozen for later transfer or donated to other couples, or used in research.
Gamete Intrafallopian Transfer (GIFT):
Overcomes low success rate of IVF.
Eggs and sperm are placed in uterine tubes immediately after being brought together.
One-step procedure for woman.
Variation: fertilize eggs in a laboratory before placing zygotes in uterine tubes.
Sexually Transmitted Diseases
Abstinence is the most effective way to prevent the spread of STDs.
Latex condoms provide some protection for those who are sexually active.
AIDS and genital herpes are caused by viruses and are not curable, but treatment is available.
STDs caused by bacteria, such as chlamydia, gonorrhea, and syphilis, can be cured with antibiotics.
STD’s Caused by Viruses
AIDS is caused by HIV, which attacks helper T cells.
AIDS has three stages: categories A, B, and C.
Category A: asymptomatic carrier can pass on the infection.
Category B: lymph nodes swell, weight loss, night sweats, fatigue, fever, diarrhea, infections such as thrush and herpes recur.
Category C: full-blown AIDS characterized by nervous disorders and the development of an opportunistic disease.
HPV is a retrovirus that causes warts, including genital warts.
10 types of HPV can cause cervical cancer.
HPV vaccine Gardasil is effective against the four most common types of HPV found in the United States.
Genital herpes is characterized by painful blisters on the genitals.
Hepatitis is an infection of the liver and can lead to liver failure, liver cancer, and death.
Hepatitis A is usually acquired from sewage-contaminated drinking water but can also be sexually transmitted.
Hepatitis B is spread in the same manner as AIDS, but a vaccine is available.
Hepatitis C is spread when a person comes in contact with the blood of an infected person.
STDs Caused by Bacteria
Chlamydia is a bacterial infection of the lower reproductive tract.
It is usually mild or asymptomatic, especially in women.
Men may experience a mild burning sensation upon urination and a mucoid discharge.
Women may have a vaginal discharge, along with the symptoms of a urinary tract infection.
Chlamydia causes cervical ulcerations, which increase the risk of acquiring AIDS.
If misdiagnosed or left untreated, it can spread from the cervix to the uterine tubes, resulting in pelvic inflammatory disease (PID.)
PID can lead to blockage of the uterine tubes, with the possibility of sterility or infertility.
Gonorrhea is easier to diagnose in males than in females.
Males are more likely to experience painful urination and a thick, greenish-yellow urethral discharge.
A latent infection leads to PID, which affects the vasa deferentia or uterine tubes.
Inflamed tubes may become partially or completely blocked by scar tissue, resulting in sterility or infertility.
Syphilis has three stages, separated by latent periods.
During the final stage, it may affect the cardiovascular system and/or nervous system.
An infected person may become mentally retarded or blind, walk with a shuffle, or show signs of insanity.
Gummas, which are large, destructive ulcers, may develop on the skin or in the internal organs.
Syphilitic bacteria can cross the placenta, causing birth defects or stillbirth.
Syphilis is easily diagnosed with a blood test.
STDs Caused by Other Organisms
Females often have vaginitis caused by Trichomonas vaginalis or Candida albicans.
Trichomoniasis is usually acquired through sexual intercourse.
Asymptomatic males are usually the reservoir of Trichomoniasis infection.
Candida albicans is normally found in the vagina.
Candida albicans growth increases beyond normal under certain circumstances.
Women taking birth control pills are sometimes prone to yeast infections.
Antibiotics for infections elsewhere in the body can alter the normal balance of organisms in the vagina, causing a yeast infection to flare up.
29.3 Human Embryonic Development
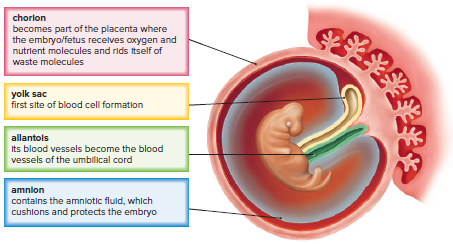
Embryonic development includes all events from fertilization to the full formation of an animal.
Humans and other mammals have similar developmental stages to all animals.
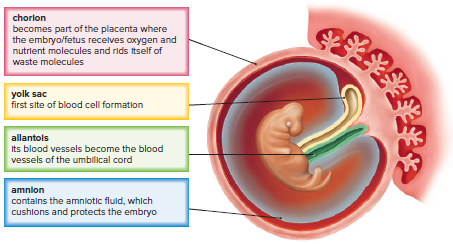
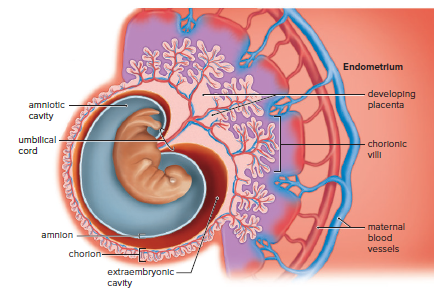
Differences exist due to extraembryonic membranes present in mammals.
These membranes protect and nourish developing mammalian embryos and fetuses in placental mammals.
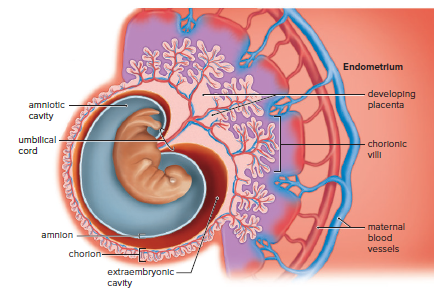
Figure 29.11 illustrates the function and identity of these membranes in mammals.
Fertilization
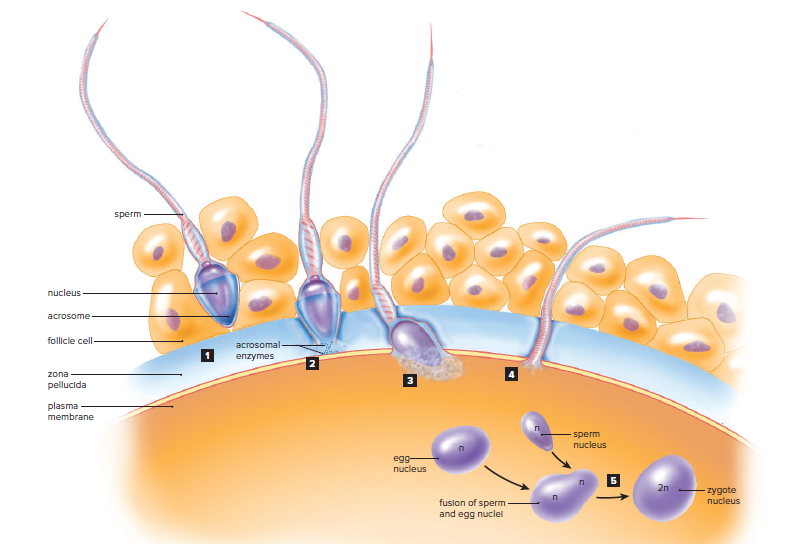
Fertilization requires interaction between sperm and secondary oocyte.
The secondary oocyte has a plasma membrane surrounded by zona pellucida and follicle cells.
Sperm releases acrosomal enzymes to digest through zona pellucida.
Sperm binds and fuses with the secondary oocyte's plasma membrane.
The secondary oocyte completes meiosis II and becomes an egg.
Haploid egg and sperm nuclei fuse.
Only one sperm should fertilize an egg to avoid too many chromosomes and non-viable zygote.
Changes in zona pellucida prevent polyspermy.
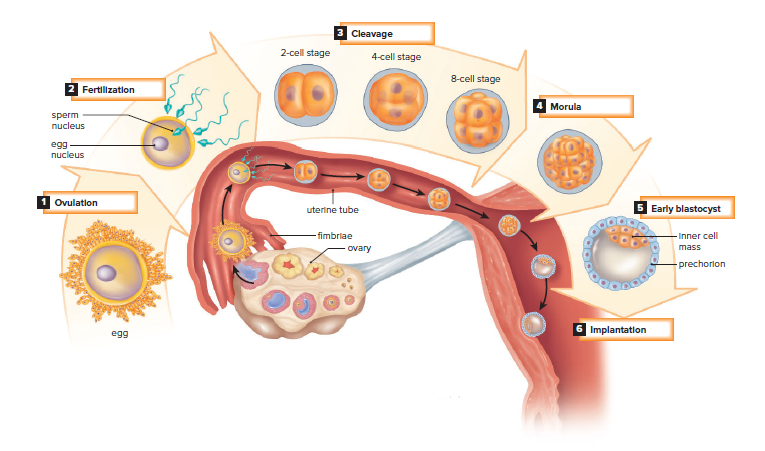
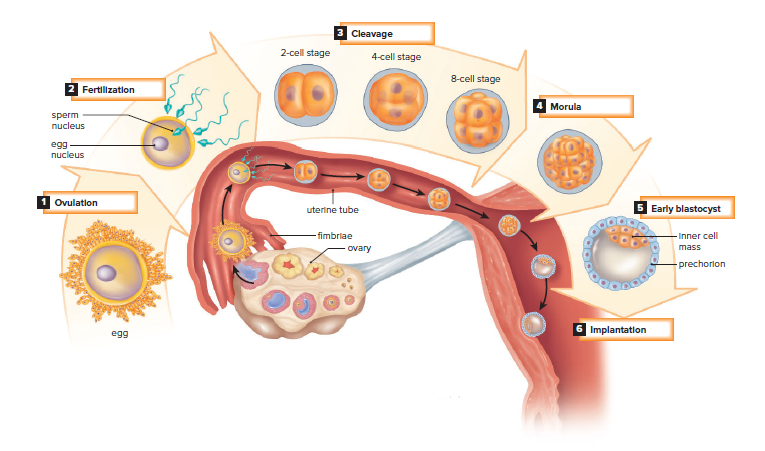
Early Embryonic Development
The first two months of development are the embryonic period.
6 days of development occur in the uterine tube before implantation.
Following fertilization, the zygote undergoes cleavage, which is cell division without growth.
Cleavage only increases the number of cells, not the original volume of the egg cytoplasm.
The resulting ball of cells is called a morula.
The morula cells secrete fluid into the center, forming a hollow ball of cells called the blastocyst.
The blastocyst has an inner cell mass that will become the embryo and an outer layer of cells that will become the chorion.
The chorion is the extraembryonic membrane that contributes to the development of the placenta.
The placenta begins to form and secrete hCG as the embryo implants in the endometrium.
hCG maintains the corpus luteum and endometrium until estrogen and progesterone take over.
Ovulation and menstruation do not occur during pregnancy.
Later Embryonic Development
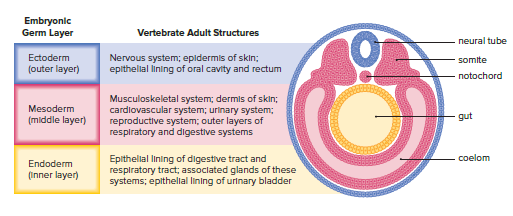
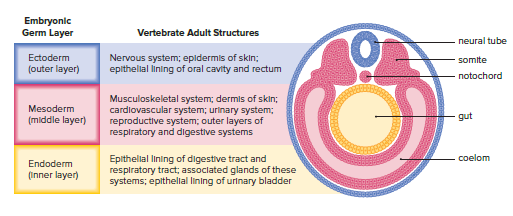
Gastrulation:
The major event that turns inner cell mass into embryonic disk.
Example of morphogenesis where cells move/migrate to become tissue layers called germ layers.
Embryonic disk becomes embryo with three primary germ layers: ectoderm, mesoderm, and endoderm.
Ectoderm, mesoderm, and endoderm are called embryonic germ layers.
Organs of animal's body develop from these three germ layers.
Neurulation:
The central nervous system is the first to form.
Mesoderm cells form a dorsal supporting rod called the notochord.
The neural plate thickens along the dorsal surface of the embryo.
Neural folds develop on both sides of the neural groove, which becomes a neural tube when folds fuse.
The anterior portion of the neural tube becomes the brain, and the posterior portion becomes the spinal cord.
Midline mesoderm cells become two masses of tissue, which are blocked off into somites.
Somites give rise to vertebrae and muscles associated with the axial skeleton.
Mesoderm splits and forms the mesodermal lining of the coelom.
The neural crest consists of a band of cells that develops where the neural tube pinches off from the ectoderm.
Cells migrate to various locations, where they contribute to the formation of skin and muscles, the adrenal medulla, and the ganglia of the peripheral nervous system.
The embryo is about 2mm long at the end of the third week, with over a dozen somites evident and the development of blood vessels and the gut.
Organ Formation Continues
At 5 weeks, the human embryo has limb buds called flippers.
Arms and legs develop from limb buds, and hands and feet become apparent.
Head enlarges, and sense organs become more prominent during the fifth week.
The umbilical cord develops from a bridge of the mesoderm called the body stalk.
The body stalk connects the caudal end of the embryo with the chorion.
The allantois, a fourth extraembryonic membrane, is contained within the stalk.
Blood vessels of the allantois become the umbilical blood vessels.
The head and tail lift up as the body stalk moves anteriorly by constriction.
The umbilical cord connects the developing embryo to the placenta.
From the sixth to eighth week, the embryo becomes easily recognized as human.
Concurrent with brain development, the neck region develops, making the head distinct from the body.
The nervous system is developed enough to permit reflex actions.
At the end of this period, the embryo is about 38 mm (1.5 in) long and weighs no more than an aspirin tablet, even though all its organ systems are established.
Placenta
The placenta has a fetal side contributed by the chorion and a maternal side consisting of uterine tissues.
The chorion has tree-like projections called chorionic villi.
Maternal and fetal blood never mix; exchange always takes place across the walls of the villi.
Carbon dioxide and other wastes move from the fetal side to the maternal side, and nutrients and oxygen move from the maternal side to the fetal side.
The umbilical cord stretches between the placenta and the fetus.
The umbilical blood vessels are an extension of the fetal circulatory system.
Harmful chemicals can cross the placenta, which is of particular concern during the embryonic period.
Each organ or part has a sensitive period during which a substance can alter its normal development.
Thalidomide, a tranquilizer, can cause limb deformities if taken between days 27 and 40 of pregnancy.
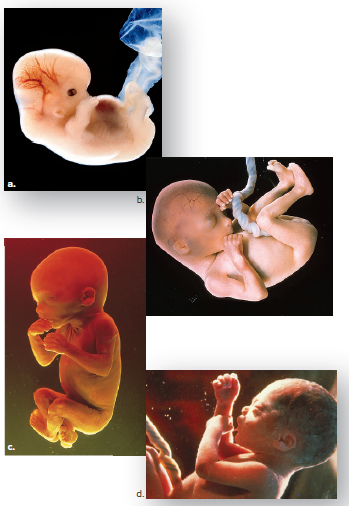
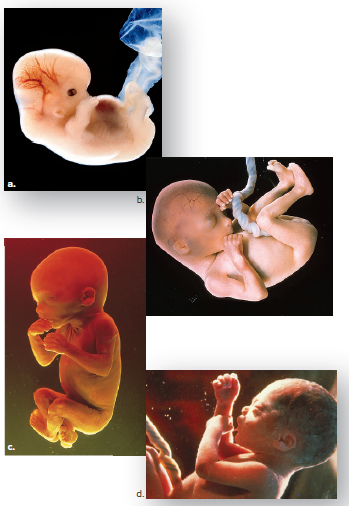
Fetal Development and Birth
Fetal development occurs from the third to the ninth month.
The fetus experiences a significant increase in size, going from less than 28 grams to approximately 3 kilograms in weight and about 50 centimeters in length.
Genitalia appears in the third month, allowing for the identification of the fetus's sex.
Hair, eyebrows, eyelashes, fingernails, and toenails develop during the third to seventh months.
A fine, downy hair called lanugo covers the limbs and trunk during the fifth to seventh months but disappears later.
The skin wrinkles due to rapid growth but is protected by a substance called vernix caseosa.
The fetus begins to move its limbs, and other systems of the body start to function.
The fetal heartbeat can be heard through a stethoscope as early as 10 weeks.
A fetus born at 22 weeks has a chance of surviving, but the lungs are often immature and cannot capture oxygen adequately.
Weight gain during the last couple of months increases the likelihood of survival.
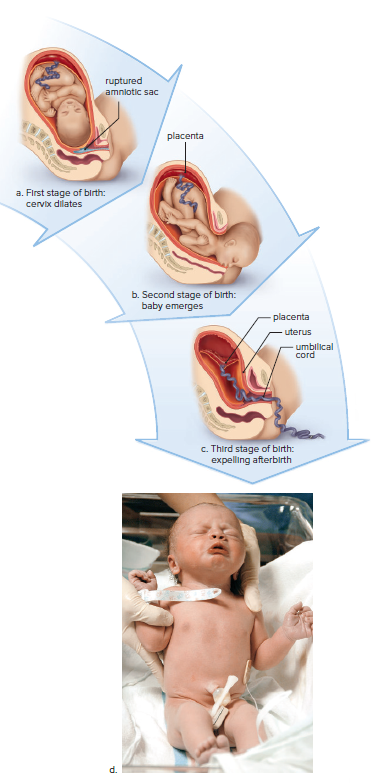
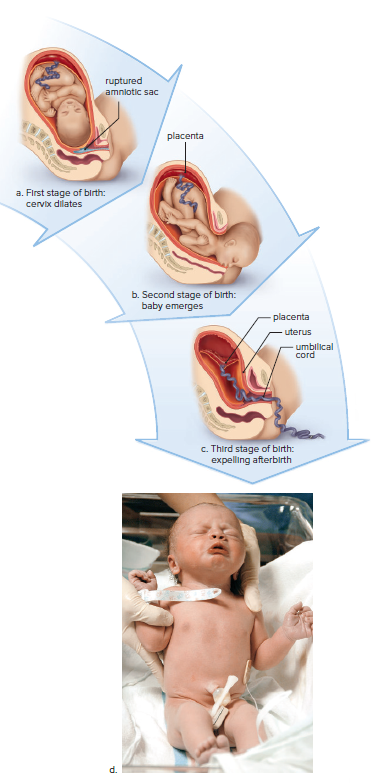
The Stages of Birth
The fetal brain matures and the hypothalamus stimulates the pituitary gland.
The pituitary gland releases androgens into the bloodstream.
The placenta uses androgens to produce estrogen.
Estrogen stimulates the production of oxytocin and prostaglandin.
Oxytocin, prostaglandin, and estrogen cause the uterus to contract and expel the fetus.
The process of birth has three stages:
First stage: the cervix dilates to allow passage of the baby's head and body.
Second stage: the baby is born and the umbilical cord is cut.
Third stage: the placenta is delivered.
Chapter 29: Reproduction and Embryonic Development
29.1 How Animals Reproduce
Asexual Versus Sexual Reproduction
Animals can reproduce sexually or asexually.
Asexual reproduction involves only one parent.
Offspring in asexual reproduction are usually genetically identical to the parent.
Sexual reproduction involves two parents.
Genetic material is shuffled in sexual reproduction.
Offspring in sexual reproduction usually have combinations of genes that are not like those of either parent.
Forms of Asexual Reproduction
Asexual reproduction occurs in hydra, a type of cnidarian.
Hydras can reproduce by budding, where a new individual arises as an outgrowth of the parent.
Many flatworms can constrict into two halves, and each half regenerates to become a new individual.
Fragmentation, followed by regeneration, is seen among sponges, echinoderms, and corals.
Chopping up a sea star does not kill it; instead, each fragment can grow into another animal if a portion of the oral disk is retained with the cut fragment.
Parthenogenesis is a modification of sexual reproduction in which an unfertilized egg develops into a complete individual.
In honeybees, the queen bee can fertilize eggs or allow eggs to pass unfertilized as she lays them.
The fertilized eggs become diploid females called workers, and the unfertilized eggs become haploid males called drones.
Parthenogenesis is also observed in some fish (including sharks) and in a number of amphibian and reptile species.

Sexual Reproduction
Sexual reproduction in animals involves the production of gametes in specialized organs called gonads.
Male gonads are called testes and produce sperm, while female gonads are called ovaries and produce eggs.
Germ cells become specialized for this purpose during early development.
Fertilization usually occurs when the egg of one parent is fertilized by the sperm of another, resulting in a zygote.
Even hermaphroditic earthworms frequently undergo cross-fertilization.
In some animals, the gonads may change function due to environmental conditions.
Aquatic animals often practice external fertilization, while internal fertilization involves copulation.
Animals either produce eggs or give birth to live offspring.
Oviparous animals lay eggs that will hatch after ejection from the body, while ovoviviparous animals retain the eggs in the body until they hatch.
Viviparous animals produce living young and provide nourishment during development via the placenta and mammary glands.
The evolution of the placenta allowed the developing offspring to exchange materials with the mother internally.

29.2 Human Reproduction
The human reproductive system has two components:
Gonads (testes in males and ovaries in females) produce gametes and sex hormones.
Accessory organs conduct gametes and house the embryo/fetus in females.
Male Reproductive System
The male reproductive system includes the testes, epididymis, vas deferens, urethra, penis, seminal vesicles, prostate gland, and bulbourethral glands.
The testes produce sperm and testosterone.
The epididymis stores and matures sperm.
The vas deferens transports sperm to the ejaculatory duct.
The ejaculatory duct joins the urethra, which carries semen out of the body.
The penis is the male organ for sexual intercourse and urination.
Erection is caused by increased blood flow to the penis.
Semen is a thick, whitish fluid that contains sperm and secretions from the seminal vesicles, prostate gland, and bulbourethral glands.
Ejaculation is the expulsion of semen from the penis.
Orgasm is the climax of sexual stimulation.
The Testes
The testes are composed of lobules, each of which contains one to three seminiferous tubules.
The seminiferous tubules are where sperm are produced.
Sperm production is a process called spermatogenesis.
Spermatogenesis involves reducing the chromosome number from diploid (2n) to haploid (n).
Sertoli cells support, nourish, and regulate the production of sperm.
A sperm has three distinct parts: a head, a middle piece, and a tail.
The head contains a nucleus and an acrosome.
The acrosome contains digestive enzymes that help the sperm penetrate the egg's outer membrane.
The tail is a flagellum that allows the sperm to swim.
The middle piece contains mitochondria that produce energy for the sperm.
A normal human male ejaculates 40 million sperm per milliliter of semen.
Only 100 sperm ever reach the vicinity of the egg, and only one sperm normally enters the egg.
Hormonal Regulation in Males
The hypothalamus secretes GnRH, which stimulates the anterior pituitary to produce gonadotropic hormones.
Both males and females have two gonadotropic hormones: FSH and LH.
In males, FSH promotes spermatogenesis in the seminiferous tubules.
LH controls the production of testosterone by the interstitial cells.
Testosterone is essential for the normal development and functioning of the sexual organs and necessary for the maturation of sperm.
Testosterone brings about and maintains male secondary sex characteristics.
Males are generally taller than females and have broader shoulders and longer legs relative to trunk length.
Testosterone causes males to develop noticeable hair on the face, chest, and occasionally other regions of the body, such as the back.
Testosterone leads to the receding hairline and contributes to pattern baldness.
Testosterone is responsible for greater muscular development in males.
Female Reproductive System
The human female reproductive system includes:
Ovaries
Uterine tubes (oviducts or fallopian tubes)
Uterus
Vagina
The uterine tubes:
Extend from the ovaries to the uterus.
Have fingerlike projections called fimbriae that sweep over the ovaries.
Sweep an oocyte into the uterine tube during ovulation.
Fertilization occurs in the first one-third of the uterine tube.
The developing embryo is propelled to the uterus by ciliary movement and tubular muscle contraction.
The Uterus:
Thick-walled, muscular organ.
Size and shape of an inverted pear.
The narrow end is called the cervix.
The embryo completes its development after embedding itself in the uterine lining (endometrium.)
The vagina:
Tube at a 45° angle with the body’s vertical axis.
The mucosal lining lies in folds, allowing it to expand.
Serves as the birth canal and facilitates sexual intercourse.
The external genital organs (vulva) include:
Mons pubis.
Labia minora and labia majora.
Clitoris (homologous to the penis of males.)
Hymen (thin membrane that partially obstructs the vaginal opening and has no apparent biological function.)
The Ovaries
Oogenesis:
An oogonium in the ovary gives rise to an oocyte surrounded by epithelium, forming a primary follicle.
At birth, a female has as many as 2 million primary follicles, but the number reduces to 300,000-400,000 by puberty.
Only about 400 primary follicles ever mature and produce a secondary oocyte.
The mature follicle bursts, releasing the secondary oocyte surrounded by follicle cells, which is called ovulation.
Oogenesis is completed when and if the secondary oocyte is fertilized by a sperm.
A follicle that has lost its oocyte develops into a corpus luteum and stays inside the ovary.
If fertilization and pregnancy do not occur, the corpus luteum begins to degenerate after about 10 days.
Ovarian Cycle:
The ovarian cycle is controlled by the gonadotropic hormones FSH and LH from the anterior pituitary gland.
During the follicular phase of the cycle, FSH promotes the development of follicles that secrete estrogen.
As the blood level of estrogen rises, it exerts feedback control over FSH secretion, and ovulation occurs.
During the luteal phase of the ovarian cycle, LH promotes the development of a corpus luteum, which secretes primarily progesterone.
As the blood level of progesterone rises, it exerts feedback control over LH secretion, so that the corpus luteum begins to degenerate if fertilization does not occur.
As the luteal phase comes to an end, menstruation occurs.
Menstrual Cycle:
The female sex hormones estrogen and progesterone affect the endometrium of the uterus, causing the series of events known as the menstrual cycle.
The 28-day menstrual cycle in the nonpregnant female is divided into three phases: menstrual, proliferative, and secretory.
During the menstrual phase, female sex hormones are at a low level in the body, causing the endometrium to disintegrate and its blood vessels to rupture.
During the proliferative phase, increased production of estrogen by ovarian follicles causes the endometrium to thicken and become vascular and glandular.
Ovulation usually occurs on day 14 of the 28-day cycle.
Hormonal Regulation in Females
Estrogen and progesterone are female sex hormones.
Estrogen is essential for normal development and functioning of female reproductive organs.
Estrogen is responsible for secondary sex characteristics in females, including body hair and fat distribution.
Females have a more rounded appearance than males due to a greater accumulation of fat beneath their skin.
The pelvic girdle aligns so that females have wider hips than males, and thighs converge at a greater angle toward the knees.
Both estrogen and progesterone are required for breast development.
Menopause occurs between ages 45 and 55 and is the time when ovarian and menstrual cycles cease.
Menopause is not complete until menstruation has been absent for a year.
Control of Reproduction
Table 29.1 lists various means of birth control and their rates of effectiveness with consistent and correct usage.
Figure 29.9 illustrates some birth control devices.
Abstinence is a reliable method of birth control that also prevents sexually transmitted diseases.
Oral contraceptives contain estrogen and progesterone, which prevent ovulation and pregnancy. Women taking birth control pills should see a physician regularly due to possible side effects.
Contraceptive implants use synthetic progesterone to prevent ovulation and are available in a single capsule that remains effective for about 3 years.
Contraceptive injections are available as progesterone only or as a combination of estrogen and progesterone and can last from a few weeks to several months.
Barrier methods of birth control, such as condoms, offer some protection against sexually transmitted diseases. Female condoms consist of a large, polyurethane tube with a flexible ring that fits onto the cervix, while male condoms are a latex sheath that fits over the erect penis.
The diaphragm is a soft, latex cup with a flexible rim that lodges behind the pubic bone and fits over the cervix. Each woman must be properly fitted by a physician and used with spermicidal jelly or cream.
The cervical cap is a mini-diaphragm.
An intrauterine device (IUD) is a small piece of molded plastic that is inserted into the uterus by a physician or another qualified health-care practitioner.
Contraceptive vaccines are currently being researched, including a vaccine intended to immunize women against human chorionic gonadotropin (hCG) and a safe antisperm vaccine for women.
Emergency contraception includes approaches to birth control that can prevent pregnancy after unprotected intercourse.
The first FDA-approved medication produced for emergency contraception was a kit called Preven, which includes four synthetic progesterone pills.
Plan B One-Step is up to 89% effective in preventing pregnancy if taken within 72 hours after unprotected sex and is available without a prescription to women aged 17 and older.
Ulipristal acetate (also known as “ella”) was approved for emergency contraception in 2010 and can be taken up to 5 days after unprotected sex.
Mifepristone, also known as RU-486 or the “abortion pill,” can cause the loss of an implanted embryo by blocking the progesterone receptors of endometrial cells.

Infertility
Control of reproduction involves preventing pregnancy and treating infertility.
Infertility is the inability to produce offspring, affecting 1 in 6 couples in America.
Causes of infertility: male (40%), female (40%), or both (20%).
Low sperm count and abnormal sperm are common causes of male infertility.
A sedentary lifestyle, smoking, and alcohol consumption can lead to male infertility.
Female body weight is an important fertility factor.
Normal weight produces the hormone leptin, stimulating follicle formation in ovaries.
Overweight women may have ineffective follicles and no ovulation.
Polycystic ovary syndrome (PCOS) affects 10% of women of childbearing age.
PCOS causes many cysts but no functioning follicles, leading to no ovulation.
Blocked uterine tubes and endometriosis are other causes of female infertility.
Medical intervention can correct some causes of infertility.
Fertility drugs can stimulate ovaries and bring about ovulation.
Assisted reproductive technologies are an option for couples who cannot conceive.
Assisted Reproductive Technologies
Assisted Reproductive Technologies (ART):
Techniques used to increase chances of pregnancy.
Sperm and/or eggs are retrieved from the testes and ovaries.
Fertilization takes place in a clinical or laboratory setting.
Artificial Insemination by Donor (AID):
Sperm is placed in the vagina by a physician.
A woman can be inseminated by her partner's sperm or the donor's sperm.
Helpful for low sperm count, sperm can be collected over time and concentrated.
In Vitro Fertilization (IVF) and Intracytoplasmic Sperm Injection (ICSI):
Conception occurs outside the body in a laboratory.
Ultrasound machines are used to spot follicles in ovaries holding immature eggs.
Immature eggs retrieved using a needle.
In IVF, immature eggs are brought to maturity in glassware before adding concentrated sperm.
In ICSI, a single sperm is injected into an egg.
Embryos are transferred to the uterus of a woman in the secretory phase of the menstrual cycle.
Embryos can be tested for genetic disease before use.
Multiple births are common if several embryos are transferred.
Excess embryos may be frozen for later transfer or donated to other couples, or used in research.
Gamete Intrafallopian Transfer (GIFT):
Overcomes low success rate of IVF.
Eggs and sperm are placed in uterine tubes immediately after being brought together.
One-step procedure for woman.
Variation: fertilize eggs in a laboratory before placing zygotes in uterine tubes.
Sexually Transmitted Diseases
Abstinence is the most effective way to prevent the spread of STDs.
Latex condoms provide some protection for those who are sexually active.
AIDS and genital herpes are caused by viruses and are not curable, but treatment is available.
STDs caused by bacteria, such as chlamydia, gonorrhea, and syphilis, can be cured with antibiotics.
STD’s Caused by Viruses
AIDS is caused by HIV, which attacks helper T cells.
AIDS has three stages: categories A, B, and C.
Category A: asymptomatic carrier can pass on the infection.
Category B: lymph nodes swell, weight loss, night sweats, fatigue, fever, diarrhea, infections such as thrush and herpes recur.
Category C: full-blown AIDS characterized by nervous disorders and the development of an opportunistic disease.
HPV is a retrovirus that causes warts, including genital warts.
10 types of HPV can cause cervical cancer.
HPV vaccine Gardasil is effective against the four most common types of HPV found in the United States.
Genital herpes is characterized by painful blisters on the genitals.
Hepatitis is an infection of the liver and can lead to liver failure, liver cancer, and death.
Hepatitis A is usually acquired from sewage-contaminated drinking water but can also be sexually transmitted.
Hepatitis B is spread in the same manner as AIDS, but a vaccine is available.
Hepatitis C is spread when a person comes in contact with the blood of an infected person.
STDs Caused by Bacteria
Chlamydia is a bacterial infection of the lower reproductive tract.
It is usually mild or asymptomatic, especially in women.
Men may experience a mild burning sensation upon urination and a mucoid discharge.
Women may have a vaginal discharge, along with the symptoms of a urinary tract infection.
Chlamydia causes cervical ulcerations, which increase the risk of acquiring AIDS.
If misdiagnosed or left untreated, it can spread from the cervix to the uterine tubes, resulting in pelvic inflammatory disease (PID.)
PID can lead to blockage of the uterine tubes, with the possibility of sterility or infertility.
Gonorrhea is easier to diagnose in males than in females.
Males are more likely to experience painful urination and a thick, greenish-yellow urethral discharge.
A latent infection leads to PID, which affects the vasa deferentia or uterine tubes.
Inflamed tubes may become partially or completely blocked by scar tissue, resulting in sterility or infertility.
Syphilis has three stages, separated by latent periods.
During the final stage, it may affect the cardiovascular system and/or nervous system.
An infected person may become mentally retarded or blind, walk with a shuffle, or show signs of insanity.
Gummas, which are large, destructive ulcers, may develop on the skin or in the internal organs.
Syphilitic bacteria can cross the placenta, causing birth defects or stillbirth.
Syphilis is easily diagnosed with a blood test.
STDs Caused by Other Organisms
Females often have vaginitis caused by Trichomonas vaginalis or Candida albicans.
Trichomoniasis is usually acquired through sexual intercourse.
Asymptomatic males are usually the reservoir of Trichomoniasis infection.
Candida albicans is normally found in the vagina.
Candida albicans growth increases beyond normal under certain circumstances.
Women taking birth control pills are sometimes prone to yeast infections.
Antibiotics for infections elsewhere in the body can alter the normal balance of organisms in the vagina, causing a yeast infection to flare up.
29.3 Human Embryonic Development
Embryonic development includes all events from fertilization to the full formation of an animal.
Humans and other mammals have similar developmental stages to all animals.
Differences exist due to extraembryonic membranes present in mammals.
These membranes protect and nourish developing mammalian embryos and fetuses in placental mammals.
Figure 29.11 illustrates the function and identity of these membranes in mammals.
Fertilization
Fertilization requires interaction between sperm and secondary oocyte.
The secondary oocyte has a plasma membrane surrounded by zona pellucida and follicle cells.
Sperm releases acrosomal enzymes to digest through zona pellucida.
Sperm binds and fuses with the secondary oocyte's plasma membrane.
The secondary oocyte completes meiosis II and becomes an egg.
Haploid egg and sperm nuclei fuse.
Only one sperm should fertilize an egg to avoid too many chromosomes and non-viable zygote.
Changes in zona pellucida prevent polyspermy.
Early Embryonic Development
The first two months of development are the embryonic period.
6 days of development occur in the uterine tube before implantation.
Following fertilization, the zygote undergoes cleavage, which is cell division without growth.
Cleavage only increases the number of cells, not the original volume of the egg cytoplasm.
The resulting ball of cells is called a morula.
The morula cells secrete fluid into the center, forming a hollow ball of cells called the blastocyst.
The blastocyst has an inner cell mass that will become the embryo and an outer layer of cells that will become the chorion.
The chorion is the extraembryonic membrane that contributes to the development of the placenta.
The placenta begins to form and secrete hCG as the embryo implants in the endometrium.
hCG maintains the corpus luteum and endometrium until estrogen and progesterone take over.
Ovulation and menstruation do not occur during pregnancy.
Later Embryonic Development
Gastrulation:
The major event that turns inner cell mass into embryonic disk.
Example of morphogenesis where cells move/migrate to become tissue layers called germ layers.
Embryonic disk becomes embryo with three primary germ layers: ectoderm, mesoderm, and endoderm.
Ectoderm, mesoderm, and endoderm are called embryonic germ layers.
Organs of animal's body develop from these three germ layers.
Neurulation:
The central nervous system is the first to form.
Mesoderm cells form a dorsal supporting rod called the notochord.
The neural plate thickens along the dorsal surface of the embryo.
Neural folds develop on both sides of the neural groove, which becomes a neural tube when folds fuse.
The anterior portion of the neural tube becomes the brain, and the posterior portion becomes the spinal cord.
Midline mesoderm cells become two masses of tissue, which are blocked off into somites.
Somites give rise to vertebrae and muscles associated with the axial skeleton.
Mesoderm splits and forms the mesodermal lining of the coelom.
The neural crest consists of a band of cells that develops where the neural tube pinches off from the ectoderm.
Cells migrate to various locations, where they contribute to the formation of skin and muscles, the adrenal medulla, and the ganglia of the peripheral nervous system.
The embryo is about 2mm long at the end of the third week, with over a dozen somites evident and the development of blood vessels and the gut.
Organ Formation Continues
At 5 weeks, the human embryo has limb buds called flippers.
Arms and legs develop from limb buds, and hands and feet become apparent.
Head enlarges, and sense organs become more prominent during the fifth week.
The umbilical cord develops from a bridge of the mesoderm called the body stalk.
The body stalk connects the caudal end of the embryo with the chorion.
The allantois, a fourth extraembryonic membrane, is contained within the stalk.
Blood vessels of the allantois become the umbilical blood vessels.
The head and tail lift up as the body stalk moves anteriorly by constriction.
The umbilical cord connects the developing embryo to the placenta.
From the sixth to eighth week, the embryo becomes easily recognized as human.
Concurrent with brain development, the neck region develops, making the head distinct from the body.
The nervous system is developed enough to permit reflex actions.
At the end of this period, the embryo is about 38 mm (1.5 in) long and weighs no more than an aspirin tablet, even though all its organ systems are established.
Placenta
The placenta has a fetal side contributed by the chorion and a maternal side consisting of uterine tissues.
The chorion has tree-like projections called chorionic villi.
Maternal and fetal blood never mix; exchange always takes place across the walls of the villi.
Carbon dioxide and other wastes move from the fetal side to the maternal side, and nutrients and oxygen move from the maternal side to the fetal side.
The umbilical cord stretches between the placenta and the fetus.
The umbilical blood vessels are an extension of the fetal circulatory system.
Harmful chemicals can cross the placenta, which is of particular concern during the embryonic period.
Each organ or part has a sensitive period during which a substance can alter its normal development.
Thalidomide, a tranquilizer, can cause limb deformities if taken between days 27 and 40 of pregnancy.
Fetal Development and Birth
Fetal development occurs from the third to the ninth month.
The fetus experiences a significant increase in size, going from less than 28 grams to approximately 3 kilograms in weight and about 50 centimeters in length.
Genitalia appears in the third month, allowing for the identification of the fetus's sex.
Hair, eyebrows, eyelashes, fingernails, and toenails develop during the third to seventh months.
A fine, downy hair called lanugo covers the limbs and trunk during the fifth to seventh months but disappears later.
The skin wrinkles due to rapid growth but is protected by a substance called vernix caseosa.
The fetus begins to move its limbs, and other systems of the body start to function.
The fetal heartbeat can be heard through a stethoscope as early as 10 weeks.
A fetus born at 22 weeks has a chance of surviving, but the lungs are often immature and cannot capture oxygen adequately.
Weight gain during the last couple of months increases the likelihood of survival.
The Stages of Birth
The fetal brain matures and the hypothalamus stimulates the pituitary gland.
The pituitary gland releases androgens into the bloodstream.
The placenta uses androgens to produce estrogen.
Estrogen stimulates the production of oxytocin and prostaglandin.
Oxytocin, prostaglandin, and estrogen cause the uterus to contract and expel the fetus.
The process of birth has three stages:
First stage: the cervix dilates to allow passage of the baby's head and body.
Second stage: the baby is born and the umbilical cord is cut.
Third stage: the placenta is delivered.
 Knowt
Knowt
