GI Tract Pathology
Pre-Knlowge of GI Tract
the diaphragm separates the esoágues from the stomach
parietal cells produce HCl and KCl (gastric acid) and excrete it in gastric glands
What happens when someone vomits for days?
hypochloremic (hyper chloride) in blood
lower pH in the stomach
PAS staining
Staines the lining of the mucus → polysaccharides
Bolus moves passively and actively through the esophagus( peristaltic movement)
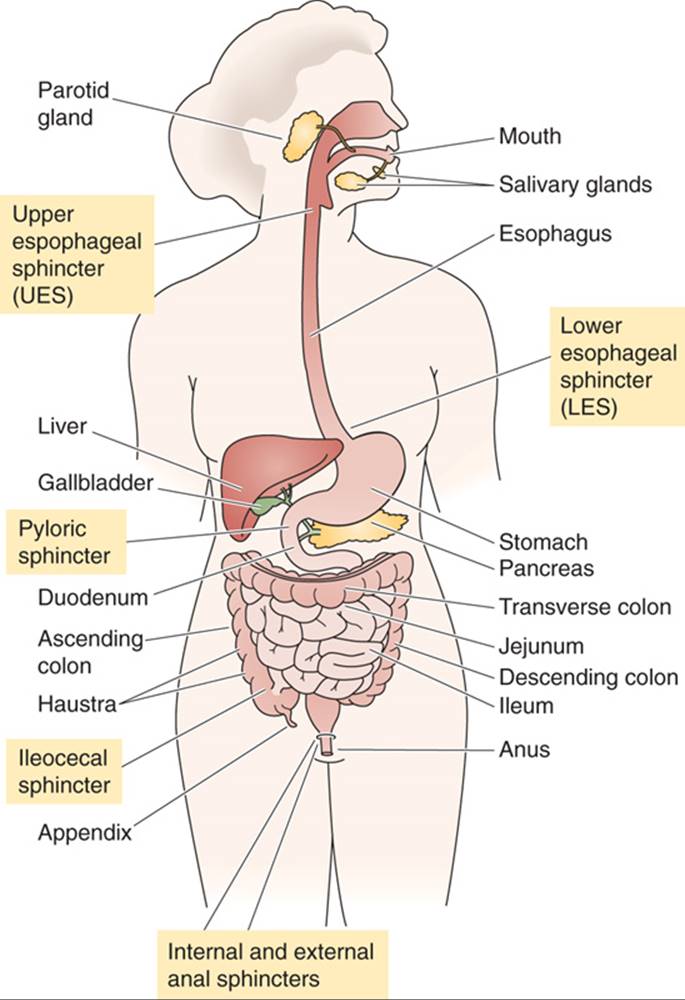
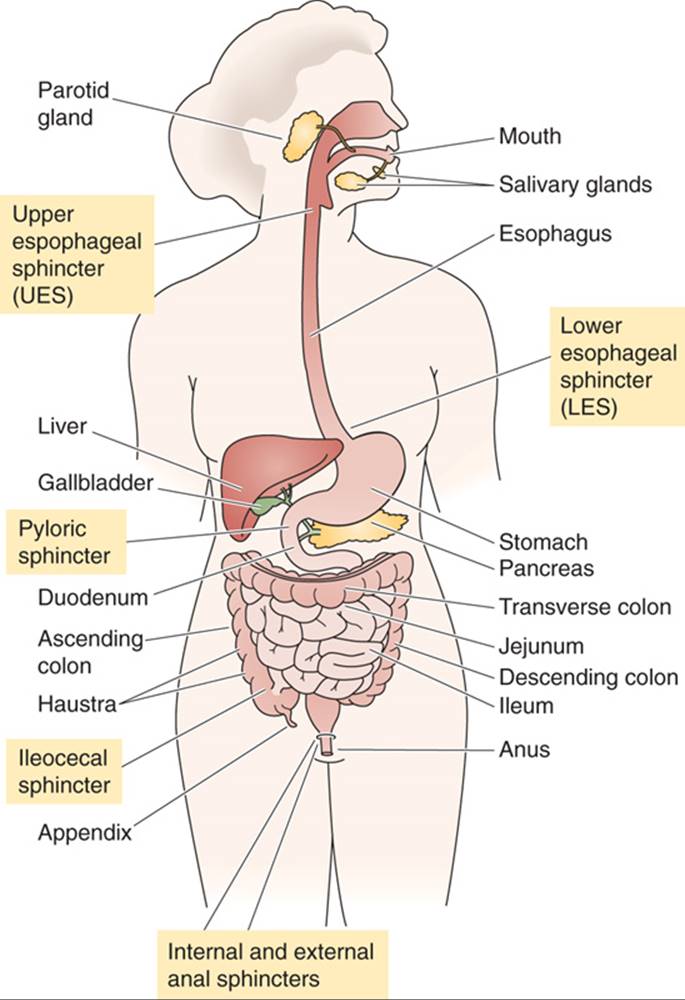
Different squinters in GI tract
Functions and Characteristics of the GI tract
Small intestines → absorption of carbohydrates, fats, minerals, proteins, water, and vitamins.
Colon: absorption of water and electrolytes
Peyers patches →patches of immune cells that are found in ilium that detect and respond to foreign substances
most bacteria found( digest found + ferment food)
Appendix: stores immune cells
GI Tract Structure | Villi* | Crypts of Lieberkuhn** | Goblet Cells*** | the cell type that lines the surface |
|---|---|---|---|---|
Esophagus | Absent | Absent | Absent | squamous cells**** |
Stomach | Absent | Present in Gastric Glands | Absent | columnar cells ***** |
Small Intestine | Present in the mucosa of the jejunum and ileum | Present | Present in the mucosa | columnar cells |
Large Intestine | Absent | Present in the mucosa | Present in the mucosa | columnar cells |
*Villi: finger-like projections on the surface of the mucosa that increase the surface area for nutrient absorption to the lymphatic system and capillaries
→ they also have mussels to move bolus muscles
**Crypts: small tube-like structures that are located in the lining of the small intestine and the large intestine, produce digestive juices + harbor stem cells for epithelial lining
***Goblet cells: goblet cells secrete mucus that protects the mucosa from damage
**** Squamous cells: are flat and often found in barrier tissues
***** Columnar cells: are taller and typically found in tissues with secretory or absorptive functions.
Pathology of esophagus
Heartburn
normally prevented by the angle of the stomach and lower esophageal sphincter(LES)
gastroesophageal reflux disease→ Barret disease of the esophagus (damaged and replaced by abnormal cells. This is usually caused by long-term acid reflux and is a risk factor for developing esophageal cancer)
Eosinophilic esophagitis
allergy in the esophagus and a lot of eosinophils → rectaion to what pathogen is unclear maybe food
IBD:
Two types of IBD (systematic disease) → due to a genetic defect, all leukocytes attack microbes and food
the peak of onset 20 and 60 → 25% of all IBD start in childhood !!!
symptoms come in waves and increase over a lifetime
loss of tolerance**
impairment of mucosal defense
epithelial barrier defects
Environmental factors:
The earlier the onset, the more genetic the IBD
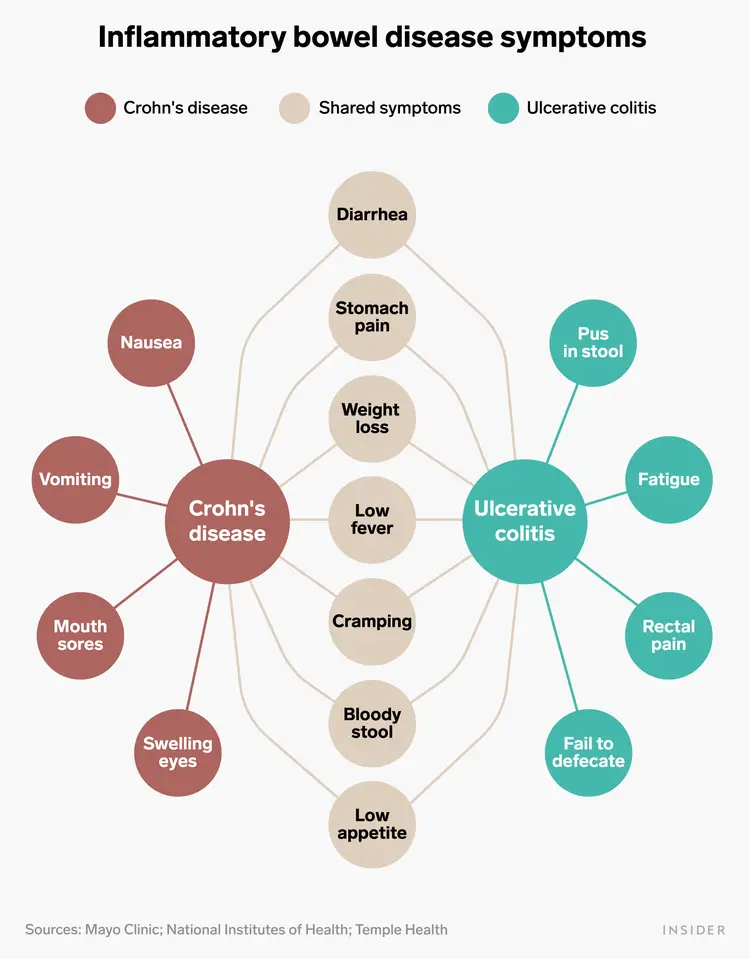
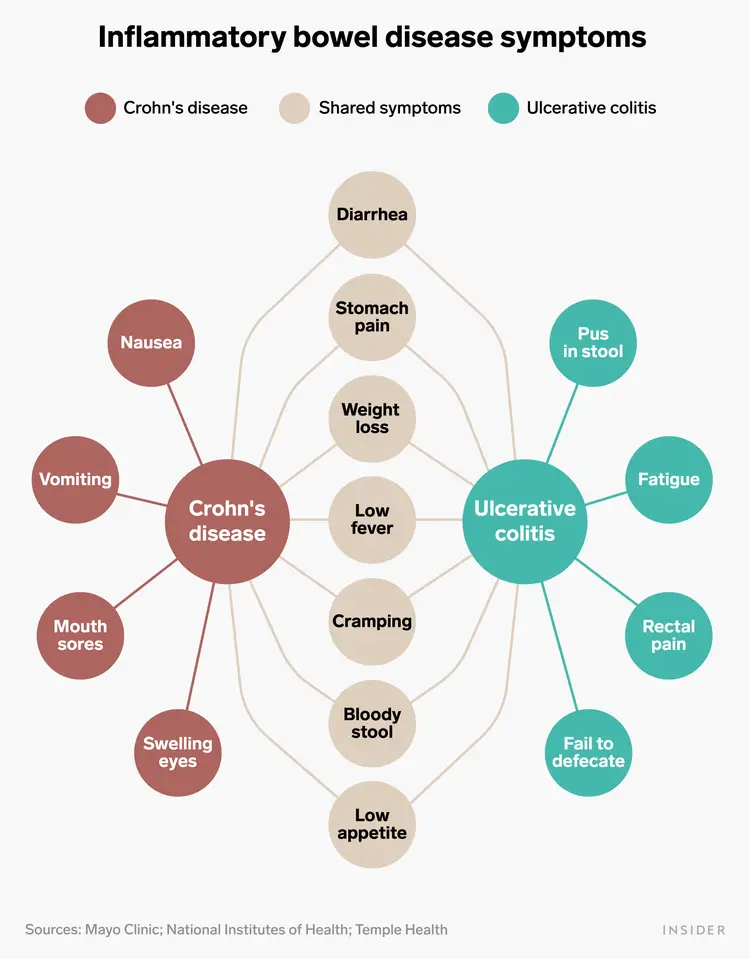
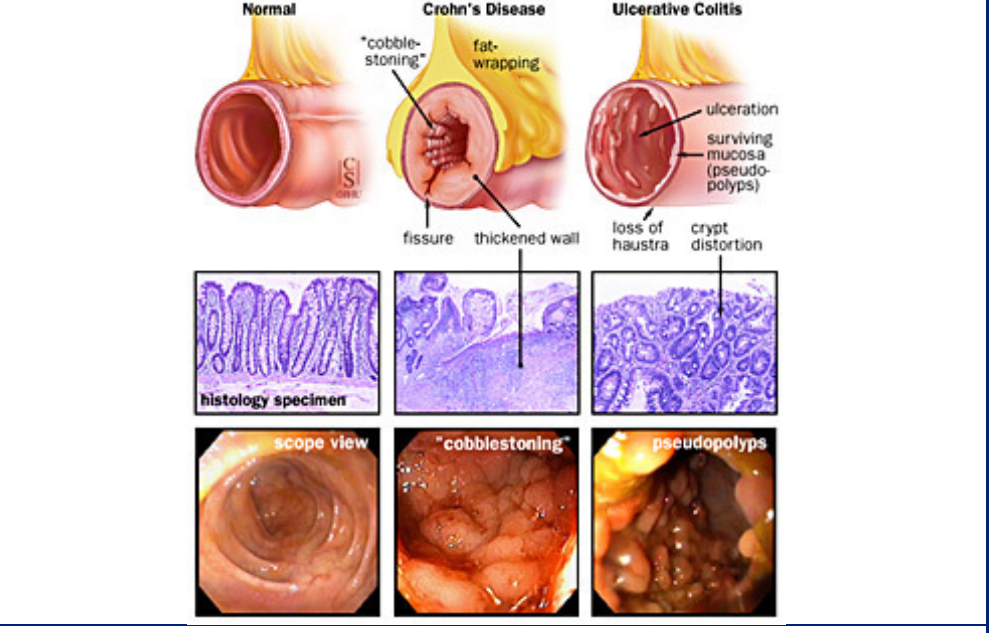
Crohn’s disease
vomiting
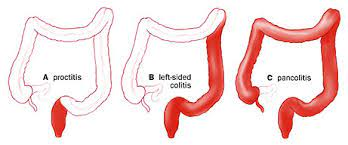
Ulcerative colitis
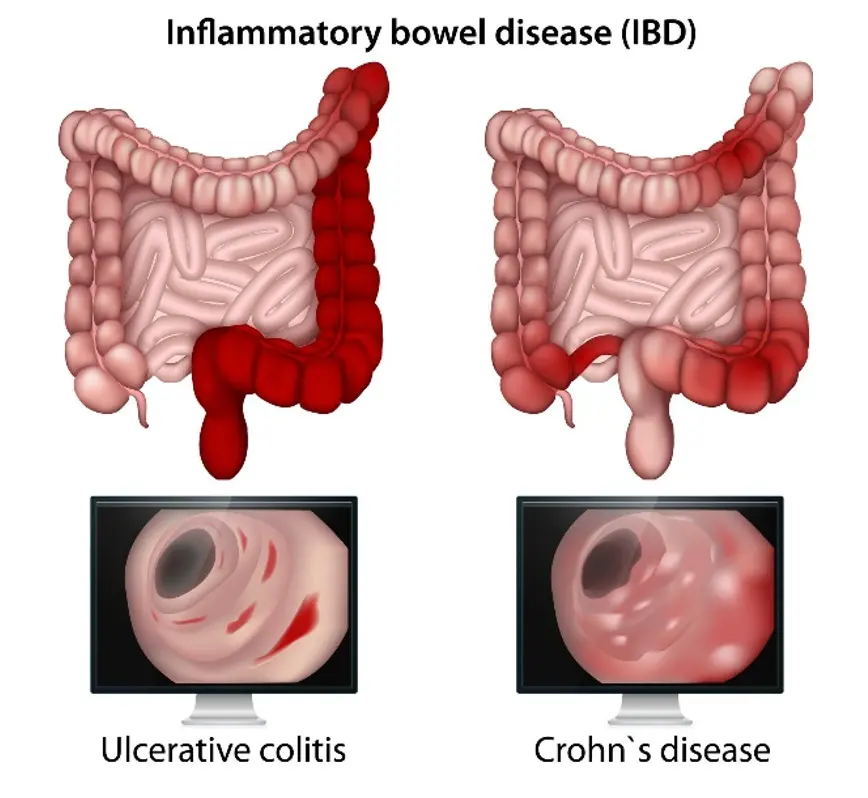
only concerns the colon → a lot of rectal symptoms that crawl upwards
(difficult to diagnose because they look so similar (diarrhea with blood+ cramping + fever), but they are very different to treat
red blood → inflammation colon
black blood → small intestine
Things that are specific to each disease
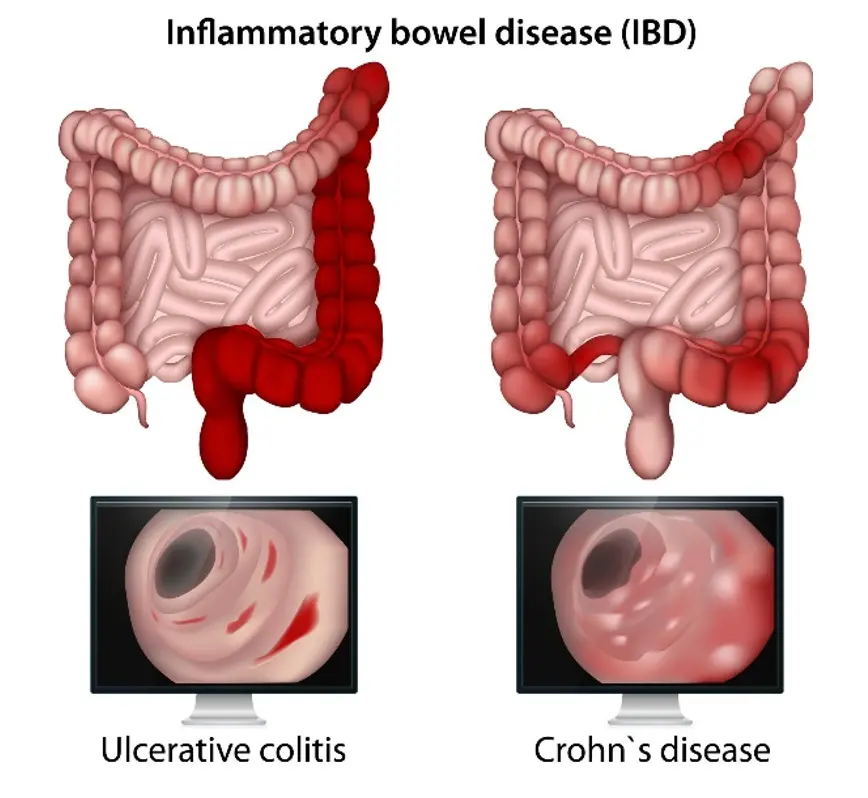
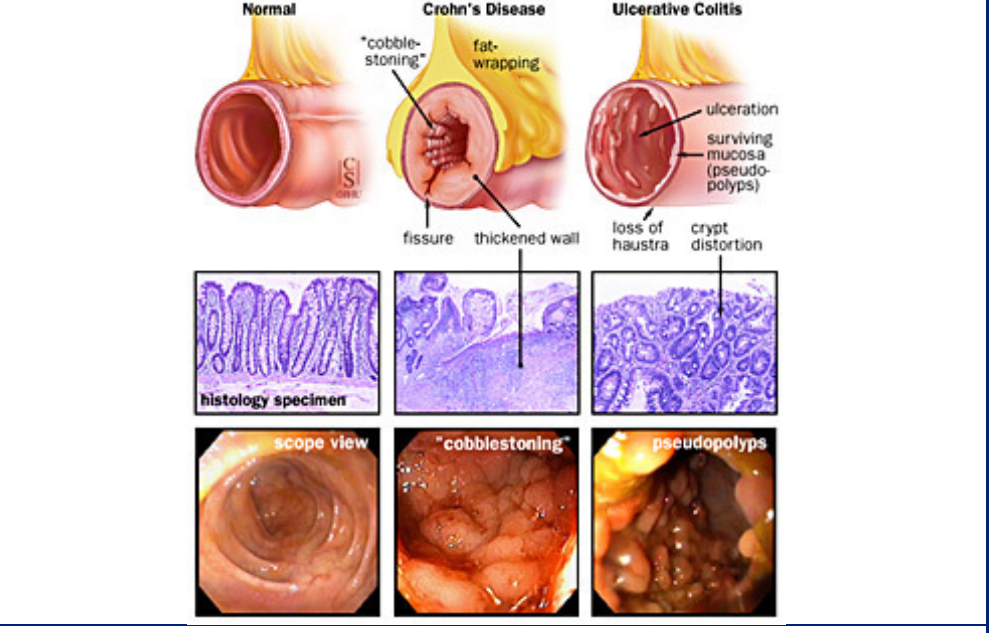
Crohn’s
the disease can skip passages in the colon and cause inflammation → patchy inflammation
Fistulas: abnormal passageways that form between different parts of the body
→ transmural ( tears through the tissue of them muscle) inflammation → feces can end up in urine
granulomas: clusters of cells that form when the body's immune system attempts to contain and eliminate foreign substances or bacteria
muscle hypertrophy
cobblestone appearance
fat wrapping
serological marker: ASCA
Ulcerative colitis
crypt distortions
always originates in the rectum and then moves up until half of the colon or the entire colon
serological markers: pANCA
ulceration within the mucosa
in children it does not have to start in rectum
Manifestation of IBD
code in the lymph node that triggers an intestine attack
you can only have skin irritation and no intestine → due to gene alteration
because innate immune system is not working( NOD 2 intracellular bacterial receptor) there is an overload of B and T cells → underlying explanation of IBD
**Tolerance in immunology
there is recognition of everything in our body by the immune system; in a normal state, there is a tolerant state; however, in IBD there is a loss of accepting new things
inflammation vs. tolerance ( too much aggressive inflammatory cells or too few protective cells)
Treatment options
take out the colon in colitis to decrease inflammation →; however, inflammation will always stay because you can’t take out return
in crohns you can’t take out the colon because inflammation will continue in small intestines
steroids
targeted immunosuppression for specific immune cells
GI Tract Pathology
Pre-Knlowge of GI Tract
the diaphragm separates the esoágues from the stomach
parietal cells produce HCl and KCl (gastric acid) and excrete it in gastric glands
What happens when someone vomits for days?
hypochloremic (hyper chloride) in blood
lower pH in the stomach
PAS staining
Staines the lining of the mucus → polysaccharides
Bolus moves passively and actively through the esophagus( peristaltic movement)
Different squinters in GI tract
Functions and Characteristics of the GI tract
Small intestines → absorption of carbohydrates, fats, minerals, proteins, water, and vitamins.
Colon: absorption of water and electrolytes
Peyers patches →patches of immune cells that are found in ilium that detect and respond to foreign substances
most bacteria found( digest found + ferment food)
Appendix: stores immune cells
GI Tract Structure | Villi* | Crypts of Lieberkuhn** | Goblet Cells*** | the cell type that lines the surface |
|---|---|---|---|---|
Esophagus | Absent | Absent | Absent | squamous cells**** |
Stomach | Absent | Present in Gastric Glands | Absent | columnar cells ***** |
Small Intestine | Present in the mucosa of the jejunum and ileum | Present | Present in the mucosa | columnar cells |
Large Intestine | Absent | Present in the mucosa | Present in the mucosa | columnar cells |
*Villi: finger-like projections on the surface of the mucosa that increase the surface area for nutrient absorption to the lymphatic system and capillaries
→ they also have mussels to move bolus muscles
**Crypts: small tube-like structures that are located in the lining of the small intestine and the large intestine, produce digestive juices + harbor stem cells for epithelial lining
***Goblet cells: goblet cells secrete mucus that protects the mucosa from damage
**** Squamous cells: are flat and often found in barrier tissues
***** Columnar cells: are taller and typically found in tissues with secretory or absorptive functions.
Pathology of esophagus
Heartburn
normally prevented by the angle of the stomach and lower esophageal sphincter(LES)
gastroesophageal reflux disease→ Barret disease of the esophagus (damaged and replaced by abnormal cells. This is usually caused by long-term acid reflux and is a risk factor for developing esophageal cancer)
Eosinophilic esophagitis
allergy in the esophagus and a lot of eosinophils → rectaion to what pathogen is unclear maybe food
IBD:
Two types of IBD (systematic disease) → due to a genetic defect, all leukocytes attack microbes and food
the peak of onset 20 and 60 → 25% of all IBD start in childhood !!!
symptoms come in waves and increase over a lifetime
loss of tolerance**
impairment of mucosal defense
epithelial barrier defects
Environmental factors:
The earlier the onset, the more genetic the IBD
Crohn’s disease
vomiting
Ulcerative colitis
only concerns the colon → a lot of rectal symptoms that crawl upwards
(difficult to diagnose because they look so similar (diarrhea with blood+ cramping + fever), but they are very different to treat
red blood → inflammation colon
black blood → small intestine
Things that are specific to each disease
Crohn’s
the disease can skip passages in the colon and cause inflammation → patchy inflammation
Fistulas: abnormal passageways that form between different parts of the body
→ transmural ( tears through the tissue of them muscle) inflammation → feces can end up in urine
granulomas: clusters of cells that form when the body's immune system attempts to contain and eliminate foreign substances or bacteria
muscle hypertrophy
cobblestone appearance
fat wrapping
serological marker: ASCA
Ulcerative colitis
crypt distortions
always originates in the rectum and then moves up until half of the colon or the entire colon
serological markers: pANCA
ulceration within the mucosa
in children it does not have to start in rectum
Manifestation of IBD
code in the lymph node that triggers an intestine attack
you can only have skin irritation and no intestine → due to gene alteration
because innate immune system is not working( NOD 2 intracellular bacterial receptor) there is an overload of B and T cells → underlying explanation of IBD
**Tolerance in immunology
there is recognition of everything in our body by the immune system; in a normal state, there is a tolerant state; however, in IBD there is a loss of accepting new things
inflammation vs. tolerance ( too much aggressive inflammatory cells or too few protective cells)
Treatment options
take out the colon in colitis to decrease inflammation →; however, inflammation will always stay because you can’t take out return
in crohns you can’t take out the colon because inflammation will continue in small intestines
steroids
targeted immunosuppression for specific immune cells
 Knowt
Knowt