
Chapter 25: The Urinary System
Physical Characteristics of Urine
Urinalysis (urine analysis) often provides clues to renal disease.
This yellow pigment is urochrome.
The virtual absence of urine production is termed anuria.
Excessive urine production is polyuria, which may be due to diabetes mellitus or diabetes insipidus.
Laboratories can now measure urine osmolarity directly, which is a more accurate indicator of urinary solutes than specific gravity.
Leukocyte esterase is released by leukocytes; if detected in the urine, it can be taken as indirect evidence of a urinary tract infection (UTI).
Gross Anatomy of Urine Transport

The urethra transports urine from the bladder to the outside of the body for disposal.
The urethra in both males and females begins inferior and central to the two ureteral openings forming the three points of a triangular-shaped area at the base of the bladder called the trigone (Greek tri- = “triangle” and the root of the word “trigonometry”).
Voiding is regulated by an involuntary autonomic nervous system-controlled internal urinary sphincter, consisting of smooth muscle and voluntary skeletal muscle that forms the external urinary sphincter below it.
The bladder is partially retroperitoneal (outside the peritoneal cavity) with its peritoneal-covered “dome” projecting into the abdomen when the bladder is distended with urine.
The bladder is a highly distensible organ comprised of irregular crisscrossing bands of smooth muscle collectively called the detrusor muscle.
Micturition is a less-often used, but proper term for urination or voiding.
Voluntary micturition requires an intact spinal cord and functional pudendal nerve arising from the sacral micturition center.
Gross Anatomy of the Kidney
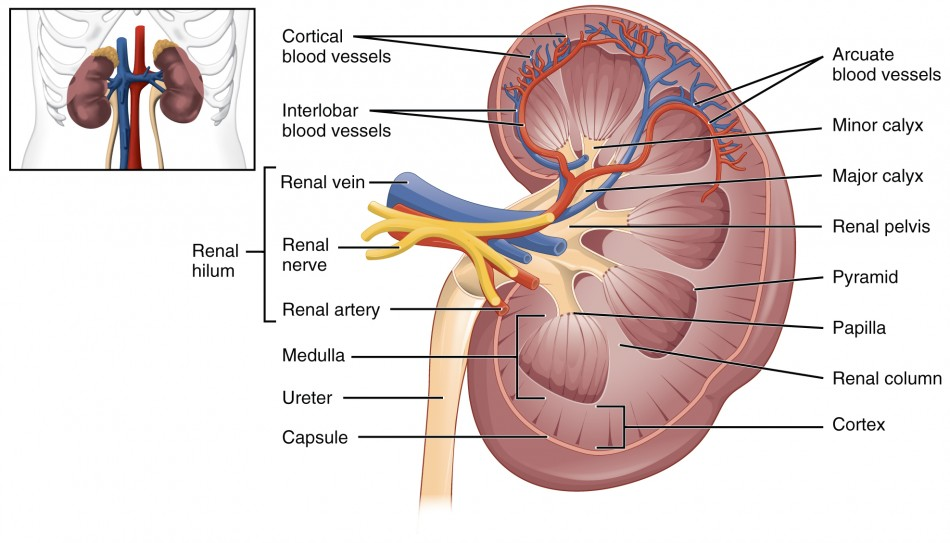
The kidneys are slightly protected by the ribs and are surrounded by fat for protection.
A frontal section through the kidney reveals an outer region called the renal cortex and an inner region called the medulla.
The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae.
The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters.
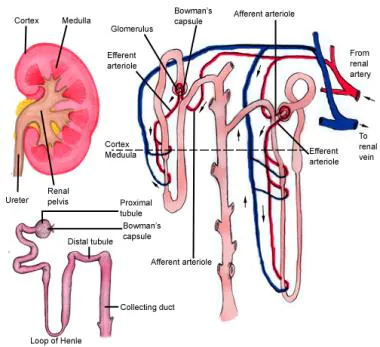
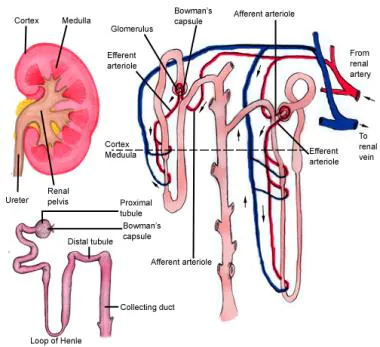
Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation.
The glomerulus and Bowman’s capsule together form the renal corpuscle.
Some nephrons have a short loop of Henle that does not dip beyond the cortex.
About 15 percent of nephrons have long loops of Henle that extend deep into the medulla and are called juxtamedullary nephrons.
Microscopic Anatomy of the Kidney
The term forming urine will be used hereafter to describe the filtrate as it is modified into true urine.
The fenestrations prevent filtration of blood cells or large proteins, but allow most other constituents through.
Lying just outside Bowman’s capsule and the glomerulus is the juxtaglomerular apparatus (JGA).
There are also mesangial cells in the filtration membrane that can contract to help regulate the rate of filtration of the glomerulus.
The wall of the DCT at that point forms a part of the JGA known as the macula densa.
A second cell type in this apparatus is the juxtaglomerular cell.
Angiotensin I is not biologically active until converted to angiotensin II by angiotensin-converting enzyme (ACE) from the lungs.
Angiotensin II is a systemic vasoconstrictor that helps to regulate blood pressure by increasing it.
Physiology of Urine Formation
The volume of filtrate formed by both kidneys per minute is termed the glomerular filtration rate (GFR).
The sum of all of the influences, both osmotic and hydrostatic, results in a net filtration pressure (NFP) of about 10 mm Hg.
This “plumps up” the tissues and cells, a condition termed systemic edema.
Regulation of Renal Blood Flow
Sympathetic nerves are part of the autonomic nervous system, which is responsible for the body's involuntary functions such as digestion, heart rate, and blood pressure.
These nerves help regulate the body's response to stress and other external stimuli.
They are also involved in the regulation of the body's temperature, pupil dilation, and other physiological responses.
Autoregulation is a process by which an organism or system maintains its internal environment in a relatively constant state, regardless of external changes.
Autoregulation is an important adaptive mechanism in living organisms, allowing them to adjust to changing environmental conditions without having to constantly alter their behavior or physiology.
Autoregulation is also used in many technological systems, such as power grids and computer networks, to ensure that they remain stable and functioning even when their external conditions change.
The myogenic mechanism regulating blood flow within the kidney depends upon a characteristic shared by most smooth muscle cells of the body.
The tubuloglomerular feedback mechanism involves the JGA and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO).
Endocrine Regulation of Kidney Function
Renin is an enzyme that is produced by the granular cells of the afferent arteriole at the JGA.
Endothelins, 21-amino acid peptides, are extremely powerful vasoconstrictors.
Natriuretic hormones are peptides that stimulate the kidneys to excrete sodium an effect opposite that of aldosterone.
Parathyroid hormone (PTH) is an 84-amino acid peptide produced by the parathyroid glands in response to decreased circulating Ca++ levels.
Regulation of Fluid Volume and Composition
A diuretic is a compound that increases urine volume.
The acid–base homeostasis of the body is a function of chemical buffers and physiologic buffering provided by the lungs and kidneys.
The parathyroid glands monitor and respond to circulating levels of Ca++ in the blood.
Chloride is important in acid–base balance in the extracellular space and has other functions, such as in the stomach, where it combines with hydrogen ions in the stomach lumen to form hydrochloric acid, aiding digestion.
Water-soluble drugs may be excreted in the urine and are influenced by one or all of the following processes: glomerular filtration, tubular secretion, or tubular reabsorption.
The Urinary System and Homeostasis
Vitamin D Synthesis: In order for vitamin D to become active, it must undergo a hydroxylation reaction in the kidney, that is, an –OH group must be added to calcidiol to make calcitriol (1,25-dihydroxycholecalciferol).
Erythropoiesis: EPO is a 193-amino acid protein that stimulates the formation of red blood cells in the bone marrow.
Regulation of Osmolarity: Blood pressure and osmolarity are regulated in a similar fashion.
Chapter 25: The Urinary System
Physical Characteristics of Urine
Urinalysis (urine analysis) often provides clues to renal disease.
This yellow pigment is urochrome.
The virtual absence of urine production is termed anuria.
Excessive urine production is polyuria, which may be due to diabetes mellitus or diabetes insipidus.
Laboratories can now measure urine osmolarity directly, which is a more accurate indicator of urinary solutes than specific gravity.
Leukocyte esterase is released by leukocytes; if detected in the urine, it can be taken as indirect evidence of a urinary tract infection (UTI).
Gross Anatomy of Urine Transport

The urethra transports urine from the bladder to the outside of the body for disposal.
The urethra in both males and females begins inferior and central to the two ureteral openings forming the three points of a triangular-shaped area at the base of the bladder called the trigone (Greek tri- = “triangle” and the root of the word “trigonometry”).
Voiding is regulated by an involuntary autonomic nervous system-controlled internal urinary sphincter, consisting of smooth muscle and voluntary skeletal muscle that forms the external urinary sphincter below it.
The bladder is partially retroperitoneal (outside the peritoneal cavity) with its peritoneal-covered “dome” projecting into the abdomen when the bladder is distended with urine.
The bladder is a highly distensible organ comprised of irregular crisscrossing bands of smooth muscle collectively called the detrusor muscle.
Micturition is a less-often used, but proper term for urination or voiding.
Voluntary micturition requires an intact spinal cord and functional pudendal nerve arising from the sacral micturition center.
Gross Anatomy of the Kidney
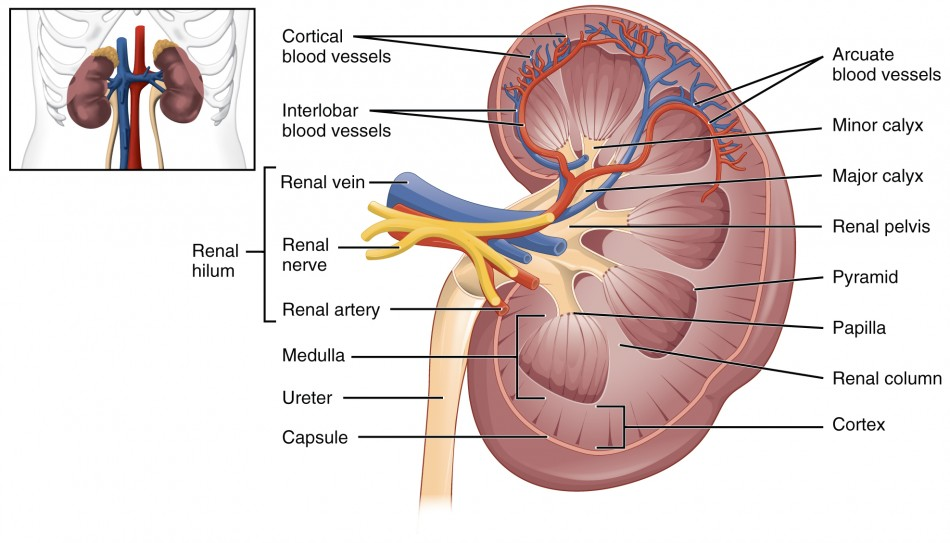
The kidneys are slightly protected by the ribs and are surrounded by fat for protection.
A frontal section through the kidney reveals an outer region called the renal cortex and an inner region called the medulla.
The renal columns are connective tissue extensions that radiate downward from the cortex through the medulla to separate the most characteristic features of the medulla, the renal pyramids and renal papillae.
The renal hilum is the entry and exit site for structures servicing the kidneys: vessels, nerves, lymphatics, and ureters.
Nephrons are the “functional units” of the kidney; they cleanse the blood and balance the constituents of the circulation.
The glomerulus and Bowman’s capsule together form the renal corpuscle.
Some nephrons have a short loop of Henle that does not dip beyond the cortex.
About 15 percent of nephrons have long loops of Henle that extend deep into the medulla and are called juxtamedullary nephrons.
Microscopic Anatomy of the Kidney
The term forming urine will be used hereafter to describe the filtrate as it is modified into true urine.
The fenestrations prevent filtration of blood cells or large proteins, but allow most other constituents through.
Lying just outside Bowman’s capsule and the glomerulus is the juxtaglomerular apparatus (JGA).
There are also mesangial cells in the filtration membrane that can contract to help regulate the rate of filtration of the glomerulus.
The wall of the DCT at that point forms a part of the JGA known as the macula densa.
A second cell type in this apparatus is the juxtaglomerular cell.
Angiotensin I is not biologically active until converted to angiotensin II by angiotensin-converting enzyme (ACE) from the lungs.
Angiotensin II is a systemic vasoconstrictor that helps to regulate blood pressure by increasing it.
Physiology of Urine Formation
The volume of filtrate formed by both kidneys per minute is termed the glomerular filtration rate (GFR).
The sum of all of the influences, both osmotic and hydrostatic, results in a net filtration pressure (NFP) of about 10 mm Hg.
This “plumps up” the tissues and cells, a condition termed systemic edema.
Regulation of Renal Blood Flow
Sympathetic nerves are part of the autonomic nervous system, which is responsible for the body's involuntary functions such as digestion, heart rate, and blood pressure.
These nerves help regulate the body's response to stress and other external stimuli.
They are also involved in the regulation of the body's temperature, pupil dilation, and other physiological responses.
Autoregulation is a process by which an organism or system maintains its internal environment in a relatively constant state, regardless of external changes.
Autoregulation is an important adaptive mechanism in living organisms, allowing them to adjust to changing environmental conditions without having to constantly alter their behavior or physiology.
Autoregulation is also used in many technological systems, such as power grids and computer networks, to ensure that they remain stable and functioning even when their external conditions change.
The myogenic mechanism regulating blood flow within the kidney depends upon a characteristic shared by most smooth muscle cells of the body.
The tubuloglomerular feedback mechanism involves the JGA and a paracrine signaling mechanism utilizing ATP, adenosine, and nitric oxide (NO).
Endocrine Regulation of Kidney Function
Renin is an enzyme that is produced by the granular cells of the afferent arteriole at the JGA.
Endothelins, 21-amino acid peptides, are extremely powerful vasoconstrictors.
Natriuretic hormones are peptides that stimulate the kidneys to excrete sodium an effect opposite that of aldosterone.
Parathyroid hormone (PTH) is an 84-amino acid peptide produced by the parathyroid glands in response to decreased circulating Ca++ levels.
Regulation of Fluid Volume and Composition
A diuretic is a compound that increases urine volume.
The acid–base homeostasis of the body is a function of chemical buffers and physiologic buffering provided by the lungs and kidneys.
The parathyroid glands monitor and respond to circulating levels of Ca++ in the blood.
Chloride is important in acid–base balance in the extracellular space and has other functions, such as in the stomach, where it combines with hydrogen ions in the stomach lumen to form hydrochloric acid, aiding digestion.
Water-soluble drugs may be excreted in the urine and are influenced by one or all of the following processes: glomerular filtration, tubular secretion, or tubular reabsorption.
The Urinary System and Homeostasis
Vitamin D Synthesis: In order for vitamin D to become active, it must undergo a hydroxylation reaction in the kidney, that is, an –OH group must be added to calcidiol to make calcitriol (1,25-dihydroxycholecalciferol).
Erythropoiesis: EPO is a 193-amino acid protein that stimulates the formation of red blood cells in the bone marrow.
Regulation of Osmolarity: Blood pressure and osmolarity are regulated in a similar fashion.
 Knowt
Knowt
